my boyfriend and i do CGM (continuous glucose monitoring) a couple times a year to check in with our metabolic health. you don't need to do this all the time, forever, to reap the benefits!
i was originally inspired to do this when i learned about the strong relationship between how our bodies handle carbohydrates/sugar and our energy levels, mood, sleep, and overall feelings of wellness or sickness throughout the day. (you can learn more about that through Dr. Casey Means, her book Good Energy, or her podcast, Levels.)
as an athlete, i'm also interested in knowing what foods provide my body continuous, slow-burning fuel (like logs on a fire) and what foods are only giving me short-term energy that burns up and leaves me feeling hungry, tired, or dissatisfied. a glucose monitor helps you identify which foods are good fuel for YOU specifically! this is why i believe CGM is an invaluable tool that everyone should have access to - whether or not you already have, or are at risk of, type 2 diabetes (a preventable metabolic disease).
how to get a CGM: you can buy this over the counter now.
you can actually get these OVER THE COUNTER NOW for about $50 each, using FSA/HSA funds!
Stelo by Dexcom / Lingo by Abbott
in north carolina, my patients can get a CGM for about $40 cash from a local pharmacy. you can call your local pharmacies directly to determine cash prices for CGMs, and then ask your personal physician to prescribe one for you. come armed with information about why this is important for you to be healthy and well - i suggest citing information on this page. you can also cite statistics on the preventable plague that is obesity and insulin resistance affecting the vast majority of Americans - i cannot imagine a reason your physician wouldn't want to support you on your quest for metabolic wellness!
prescription CGMs that i like are the Dexcom G7 and Libre 3. i've used both, and the only difference is really the manufacturer and the app. these sensors work with most smartphones, so you do NOT need to purchase a separate receiver. i generally prescribe the libre 3 because it's cheaper here.
how to place a CGM
don't mess this up! you paid good money for this device. the first time i got a cgm, it fell off in an hour, because i didn't do things right (i took my very sweaty yoga practice shortly after... in front of a fireplace...)
- apply the sensor AFTER your workout of the day - at a time when you are not bound to be getting sweaty or wet for the next 12 hours.
- wash and dry your upper arm or stomach THOROUGHLY. then wipe with an alcohol pad and let it dry completely.
- use the device applicator to plunge the needle/device into your arm or stomach (the demos on your phone will describe exactly where/how). the adhesive should stick really well at this point.
- place a tegaderm or similar bandage over the monitor. you'll still be able to scan it with your phone. leave the tegaderm/bandage on until it falls off; this will give the monitor even more time to adhere to your skin so it doesn't come off before the expiration date (usually 10-14 days).
how to use a CGM to understand your metabolic health
i like this advice from the levels page (where you can read much more in depth about using a CGM).
- Week 1: It can take a day or two for your CGM to calibrate and give you the most accurate readings. So, for the first week, focus on getting in the habit of logging your food (i tell my patients to use the FREE app MyFitnessPal, but Levels has its own app if you choose to pay the exorbitant fee). Notice how your blood glucose reacts, but don’t get too concerned over absolute values—just watch for trends.
- Week 2: Maintain your regular diet and see how your body responds. Which meals or foods trigger blood sugar spikes, and which trigger more gradual responses? “Some of my patients unconsciously begin to eat ‘better’ when they first put on a CGM,” says Anjali Dsouza, MD, founder of the District Center for Integrative Medicine. “That’s perfectly fine, but the juicy insights come when you don’t and can figure out what things, combinations of things, and contextual things will bring about spikes so you can incorporate that knowledge into your life to improve your health outcomes.”
- Week 3: Now’s the time to start experimenting to see if you can find ways to promote more stable blood glucose. Maybe you go for short walks after meals, swap your breakfast oatmeal for chia seed pudding, and add more quality protein to the beginning of every meal. Pick a few things you can realistically do for seven full days, and note what makes a positive impact.
- Week 4: Review the past week to identify which changes you can maintain benefited you most. Try to use those insights to maintain optimal glucose for an entire week.
pearls from my experiences: alcohol! sleeping! sickness! stress! alerts!
the most interesting things i learned from my time using CGM are as follows, plus some pearls for making your use of it enjoyable and not irritating.
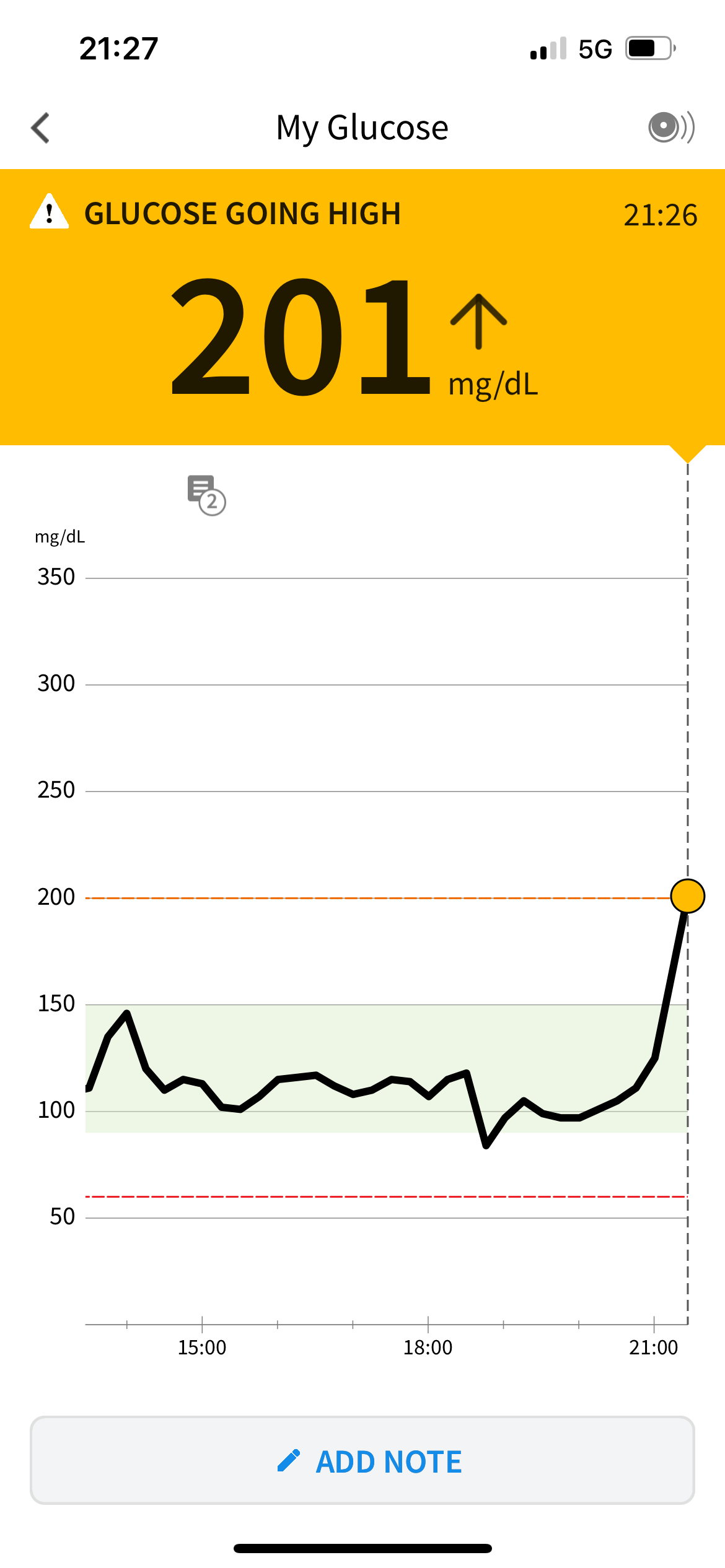
first, go change the alarms on your app to NOT alert you unless your blood sugar is below 55 mg/dL or above 130 mg/dL. the app will assume you are a type one diabetic, and need to be emergency alerted when your glucose level drops. unless you alter the alarms, you will be woken up and your phone calls and meetings will be interrupted at inopportune times.
do NOT panic when your device tells you that you are dangerously hypoglycemic and you feel just fine. my CGM routinely told me i dropped to 45 mg/dL, and although i never backed this up with a point of care blood sugar monitor, you could get one from any pharmacy to check against your CGM. friends i have who use these regularly tell me their CGM is often wrong (above or below their real blood sugar level!) by 5-15 mg/dL.
second, pay attention to what happens when you drink alcohol! it messes up your sleep big time - poor REM quality and sleep stages - and drinking before bed usually causes you to wake up a few hours into your sleep. alcohol is often sugar-laden, and it can increase insulin sensitivity, so it can cause big spikes and dips in your blood sugar levels. my biggest swings have always happened when i am out drinking, walking, dancing, and socializing - from 45 mg/dL to 110 mg/dL within an hour one evening! this is stressful for the body, and takes a toll.
third, don't be surprised when your workout leads to a big spike. high intensity activity will lead to release of catecholamines (adrenaline) and cortisol, both of which raise your blood sugar. additionally, if you are sick with an infection or illness, very stressed out, or taking steroids by mouth, your sugars can be a lot higher.
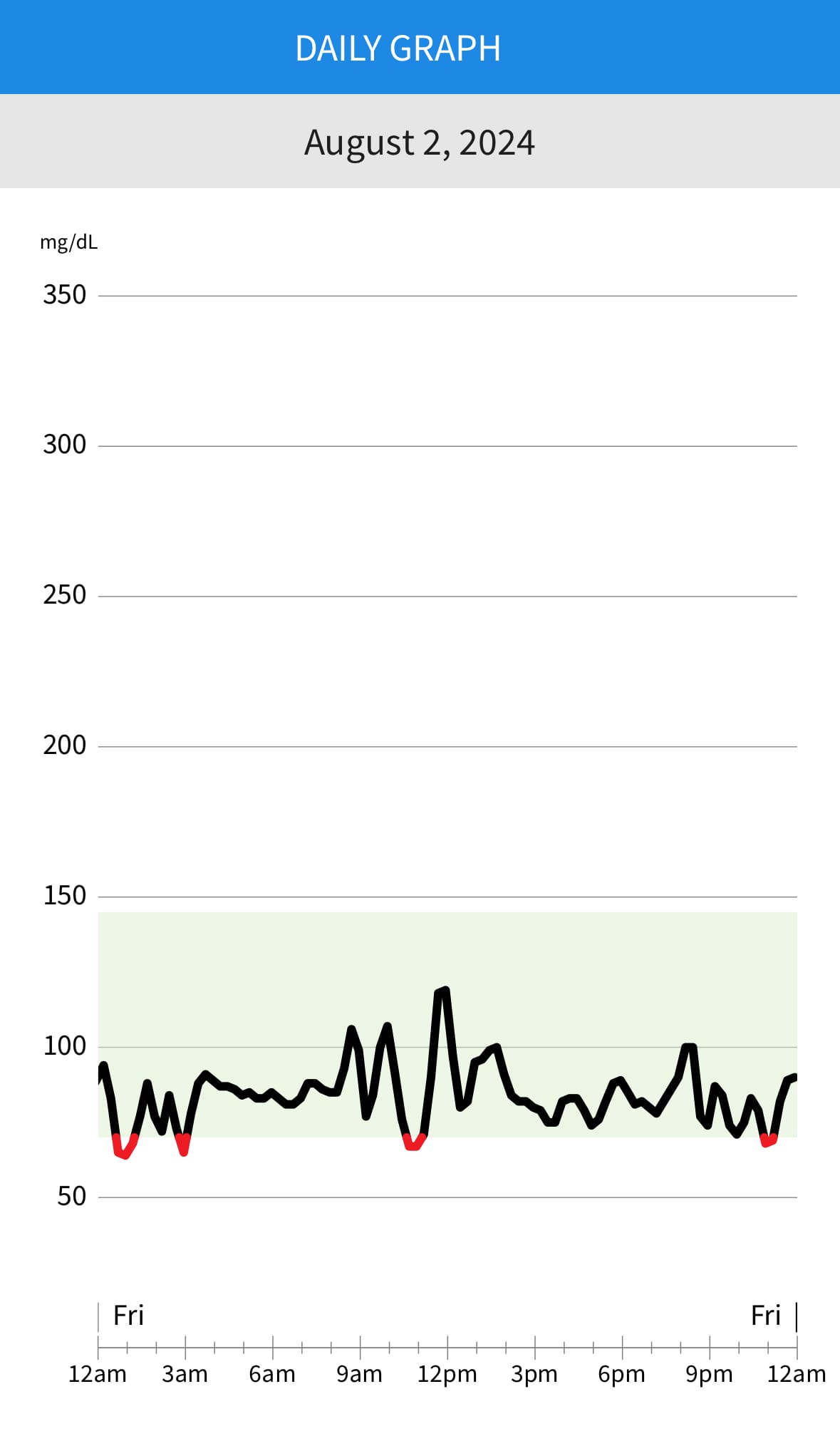
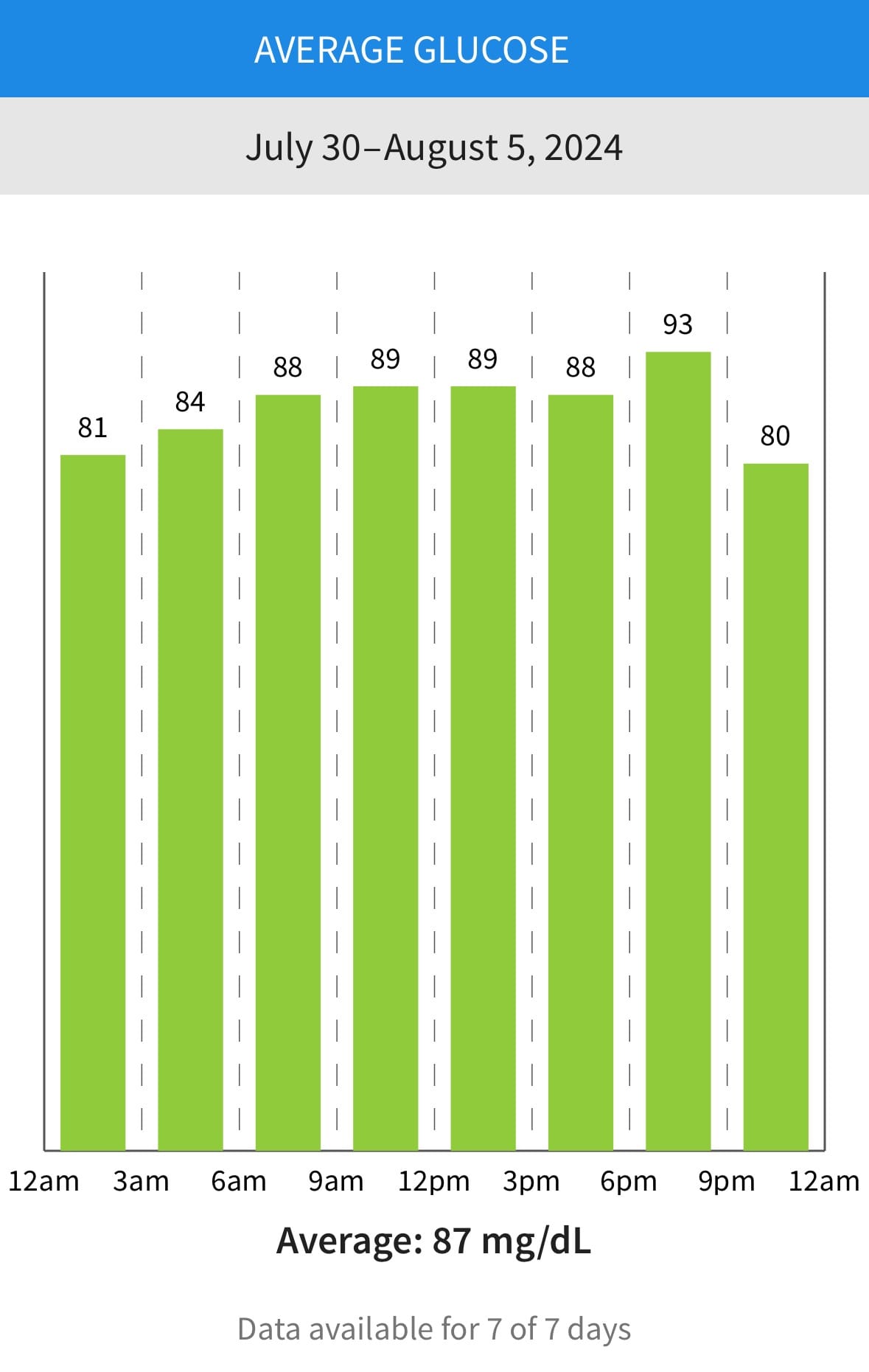
data from my CGM. notice the dips overnight, which happen pretty regularly for me (i think my muscles eat a lot of sugar at night - and this is normal!). BIG swing before lunch, possibly because i had fasted that morning - but, the spike doesn't exceed 130 mg/dL.
target levels for metabolic health
fasting: 60-80 mg/dL
generally, you want your fasting blood sugar to be between 60-80 mg/dL. a little higher is OK, but this is a good target range. pay attention to what happens right after you wake up, since this is usually a time for a small spike due to cortisol levels peaking. (cortisol is a stress hormone that helps you wake up in the morning, and increases your blood sugar levels.)
post-prandial (after meals): no more than 30 mg/dL above baseline; ideally, not above 110 mg/dL
Dr. Means states that blood sugar levels should generally not spike more than 30 mg/dL after meals. if you notice your blood sugar spikes more than that, you may have made some poor choices with your nourishment (did you drink or eat straight up sugar?). if this happens consistently, you might have some insulin resistance, and need to make meal choices accordingly! don't ever drink sugar, avoid eating too many carbohydrates, and pay attention to which carbohydrates your body tolerates (usually complex carbs, like potatoes, yucca, and beans are great options that should not spike glucose significantly).
other ways to prevent a big spike are to eat your carbs with good fats and protein, and eat your carbs AFTER eating fat and protein so they are absorbed more slowly.
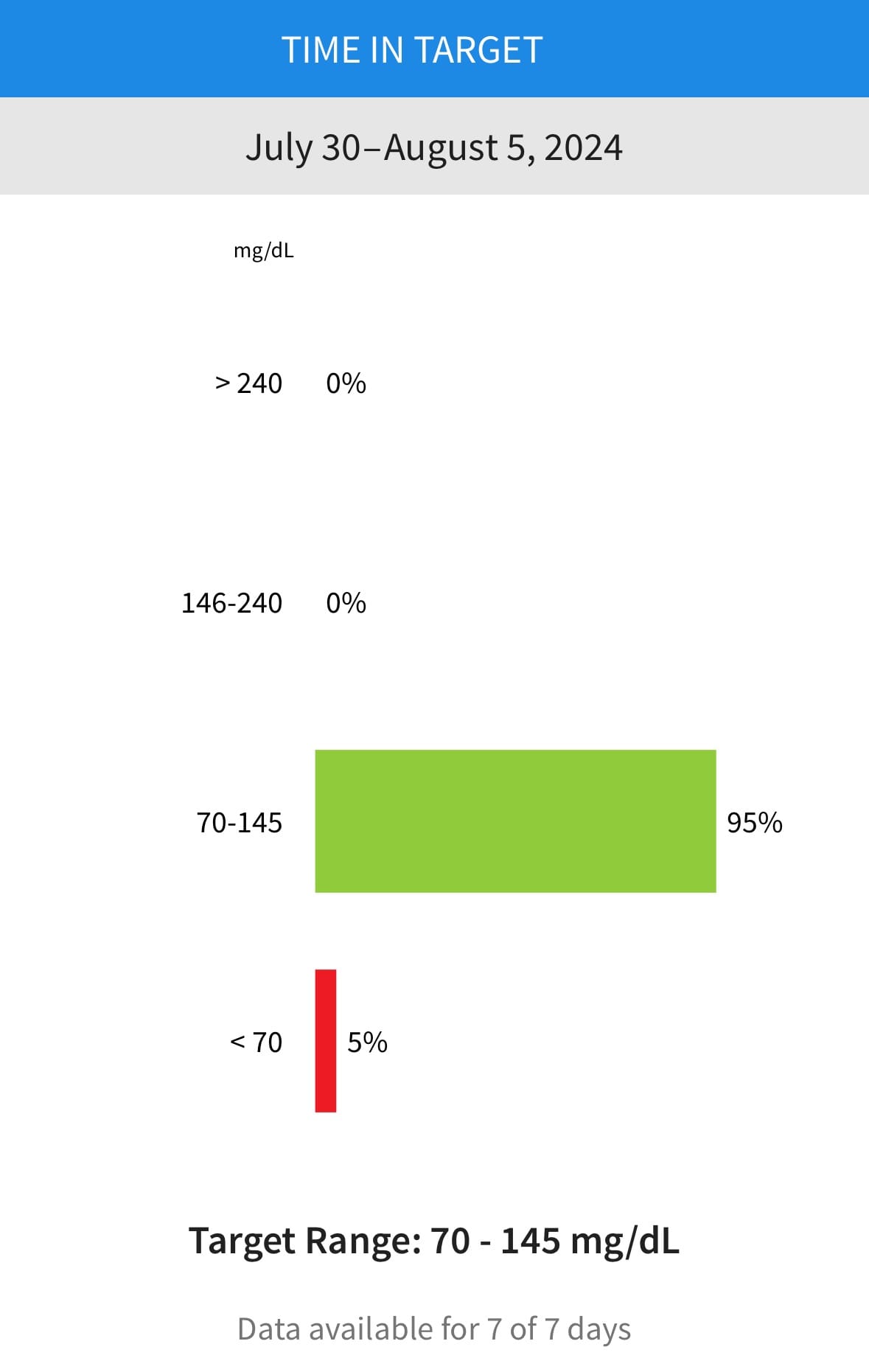
throughout the day: between 60 - 140 mg/dL (no higher or lower!)
if you are struggling to stay in this window despite using tricks like food swaps and going for walks, you might need to consider more long-term efforts to help you achieve blood sugar control. your muscles are glucose sponges, and if you have poor muscle mass, you might need to build some more quality tissue by starting strength training or weight lifting.
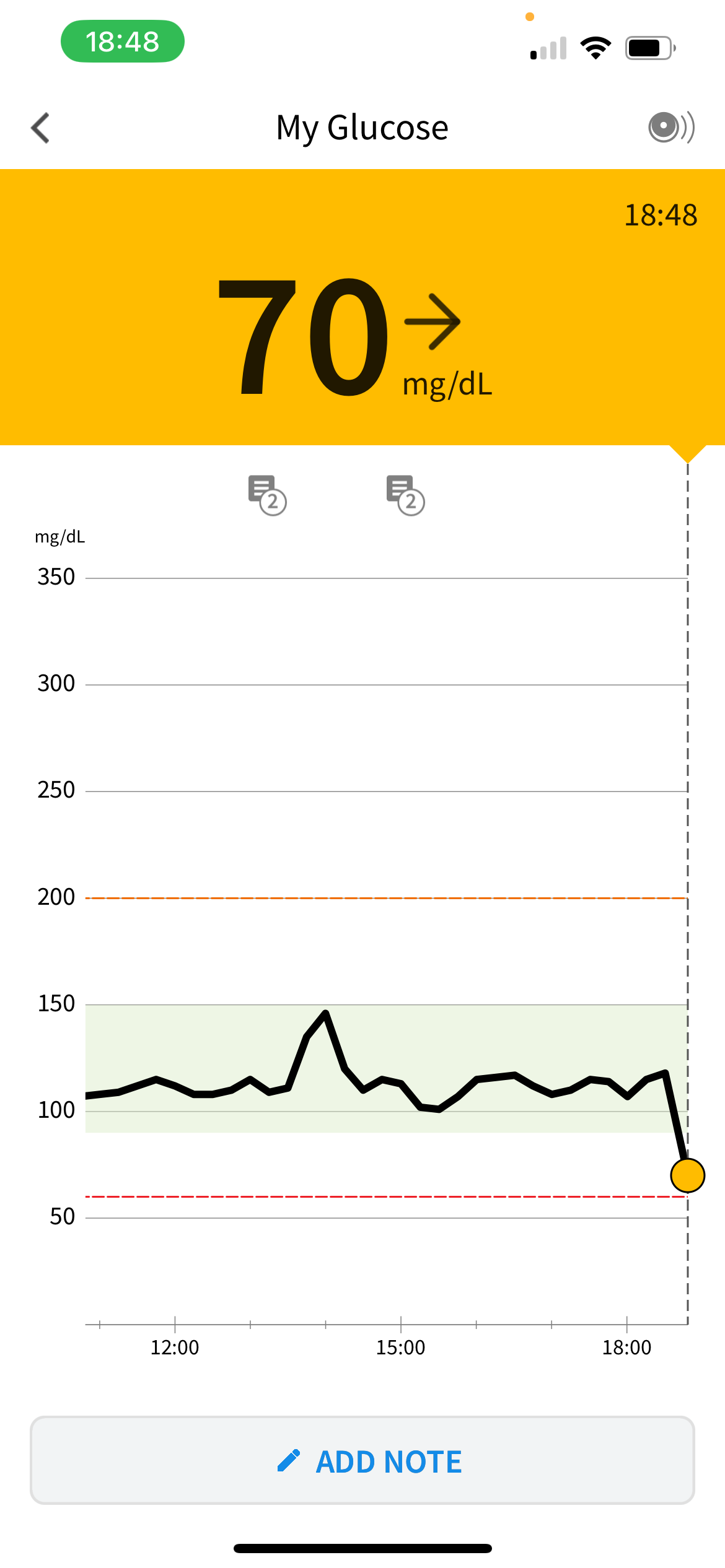
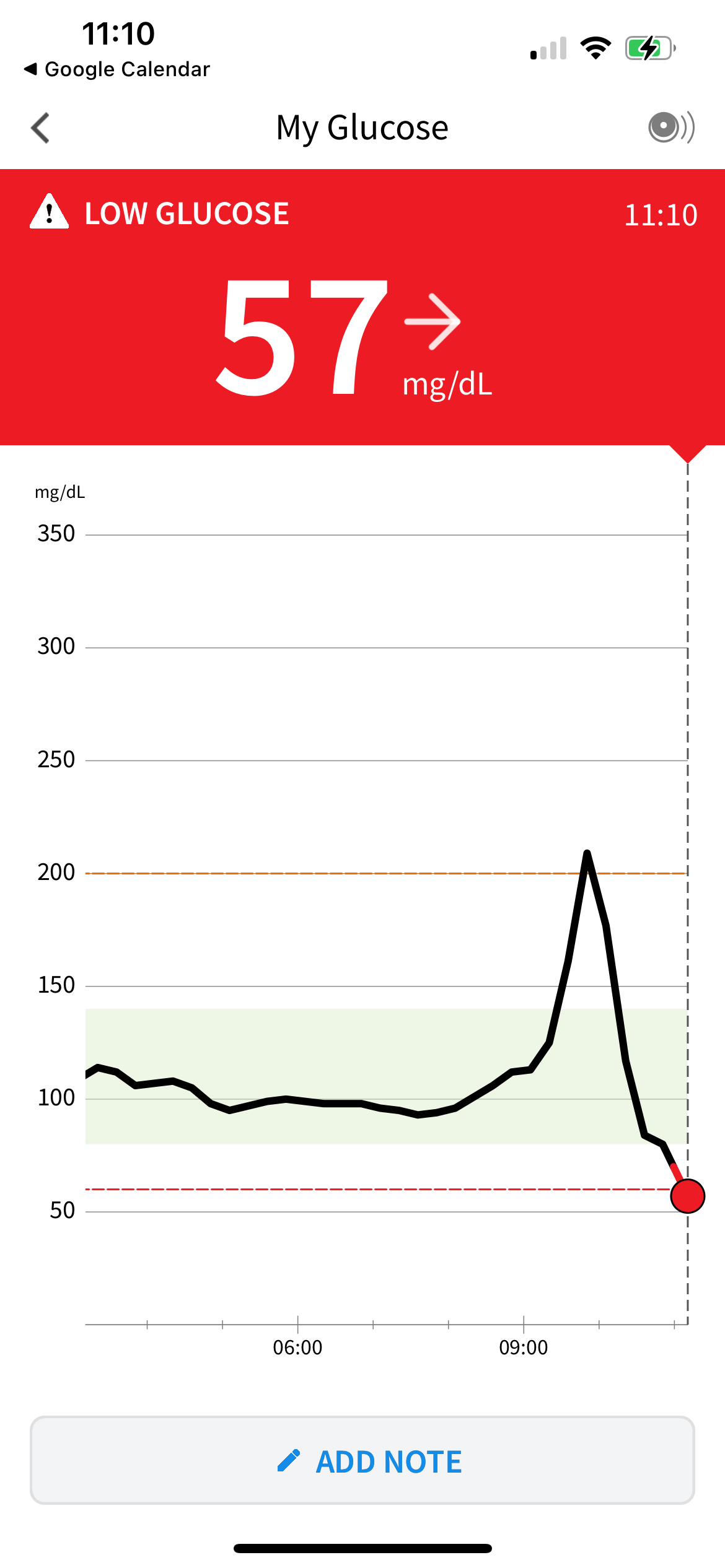
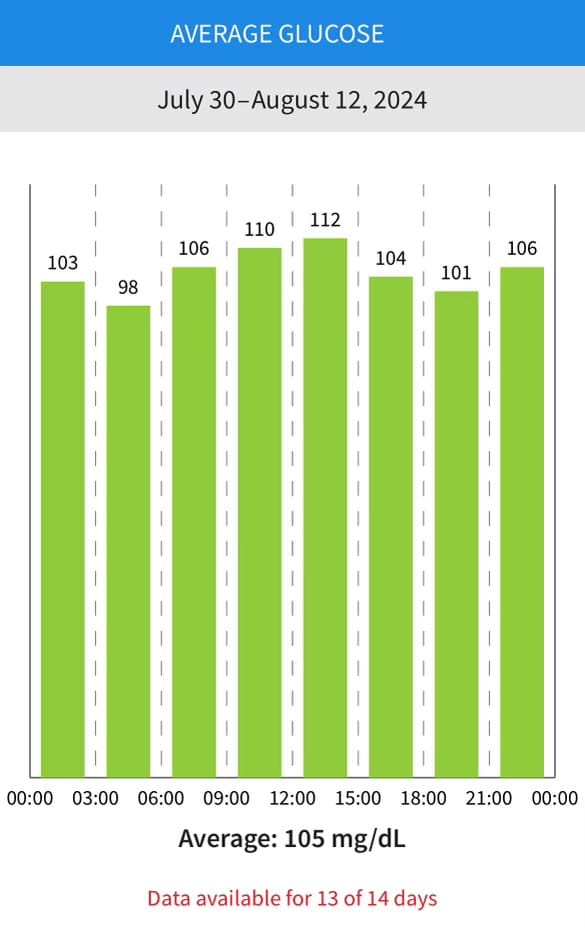
some data from my partner's CGM. the drops are all from cold plunging - submersion in 42 degree water will really drive sugar into your cells! his dramatic spike in the top right is from eating oatmeal. he stopped doing that after getting CGM, and when he does opt for overnight oats now, he mixes grains with ample protein, fat, and NO added sugar to slow the spike.